The Dumont Center for Rehabilitation and Nursing Care has received 65 total citations over the four-year period between November 2013 and October 2017, according to the New York State Department of Health. With 65 citations, the nursing home and assisted living facility in Westchester County has almost twice the number of citations for the average […]
Elder Population Studies
Rhinovirus Outbreak at Westchester Veterans Home Leaves Four Dead
In August of 2016, the New York State Veteran’s Home in Montrose, New York had a horrific rhinovirus outbreak. At one point, the facility in Westchester had one-out-of-every-four residents sick with the virus. Altogether, there were 58 documented cases of rhinovirus at the 221-bed retirement home for veterans. Sadly, four of the elderly residents with […]
New York AG: Nurse Failed to Administer Medication at Putnam Ridge Nursing and Rehabilitation Center
Attorney General Eric Schneiderman has charged a Pawling nurse with failing to administer medication to three residents at Putnam Ridge Nursing and Rehabilitation Center in Brewster, New York. Further, not only did the nurse, Stacey McAdams, fail to administer the necessary medication to the elderly residents at the nursing home, she also falsified medical records […]
Studies: Low-Quality Medicare Advantage Plans Harm Elderly
A recent study by Health Affairs shows that elderly Americans enrolled in Medicare Advantage plans are more likely to end up at a lower-quality nursing home or assisted living facility, compared to senior citizens with traditional Medicare coverage. A Medicare Advantage health insurance plan is an increasingly popular alternative to traditional Medicare plans. A Medicare […]
Government Report: 25 Percent of Nursing Home Abuse Never Reported
A scathing report by the Office of Inspector General shows that 25 percent of nursing home abuse cases go unreported. Of these unreported cases, 80 percent involved an allegation of sexual abuse or rape of an elderly person. The Center for Medicare and Medicaid Services (CMS) has promised to do more to identify abuse and […]
Report: Popularity of “Day Passes” in Nursing Homes Often Confines Residents, Limit Freedom
A report by Mobilization for Justice has shined a light on how the popular use of “day passes” at nursing home facilities have been used to confine their elderly residents and limit their freedom. Originally intended to keep track of their elderly residents, most nursing homes required patients to attain a “day pass” whenever they […]
New York: Home Care Workers Challenge State Policy, Seek More Money
In a case that could have far reaching consequences, a group of New York’s home care workers are challenging a state policy providing only thirteen-hours of pay for home care workers performing a 24-hour shift. The Department of Labor previously created the so-called “thirteen-hour rule” for home care workers to ensure they were not being […]
Trump Administration Moves to Limit Nursing Home Resident’s Access to Court System
As part of President Trump’s promise to roll-back federal regulations, the Trump administration has announced its intention to scrap a federal rule prohibiting nursing homes from requiring their residents to pursue legal claims through arbitration. In the simplest terms, arbitration is a catch-all term for a dispute-resolution that, while legally binding, does not utilize the […]
States Take Notice as Financial Abuse of the Elderly Becomes More Common
As more than 10,000 Americans join the 65-and-over club daily, financial exploitation of the elderly is becoming increasingly more common and states are making moves to protect their senior citizens. Financial abuse, one of the four types of elder abuse (the other three include sexual abuse, physical abuse and emotional abuse) involves the “illegal or […]
Drug-Resistant Bacteria on the Rise at Nursing Homes
In a new study released by Columbia University School of Nursing, a quarter of nursing homes had a “significant presence” of multidrug-resistant bacteria. The study reviewed eight prior studies, and the reported rates of drug-resistant bacteria ranged from 11 percent to a whopping 59 percent – with 27 percent the average. Multi-drug resistant bacteria are […]
New York Nursing Homes: Know Your Rights
New York Nursing Homes Cannot Tell Patients They Only Provide “Short-Term” Service According to the New York Department of Health, a growing number of New York nursing homes are illegally telling potential patients that their facility only provides short-term care. Under New York law, this is illegal – there is no such thing as a […]
New York City Comptroller Report Calls for Long-Term Planning for New York City Seniors
As the number of senior-citizens in New York City is expected to rapidly increase in the near-future, New York City Comptroller Scott Stringer is calling for a city-wide, long-term plan to meet the needs of New York’s senior population. Between 2005 and 2015, the number of senior citizens (those over the age of 65) rose […]
Six Individuals Arrested for Stealing from Nursing Home Residents
On October 18, 2016, six individuals were arrested in New York for exploiting the financial vulnerability of nursing home residents; defendants are from Bronx, New York, Queens and Suffolk Counties. The five New York City defendants stole personal identity information from residents in order to secure cash or credit they were not entitled to; and […]
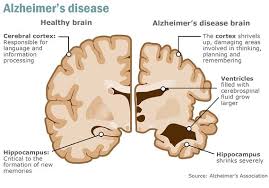
Study Suggests Cure to Alzheimer’s May Be on the Horizon
An experimental drug may have led researchers one step closer to preventing Alzheimer’s disease. The drug is called ‘aducanumab’ and was developed by Biogen, a pharmaceutical company based in Massachusetts who also funded the study; results were published on Wednesday on Nature.com. In patients with Alzheimer’s, scientists have found an abnormal structure called ‘plaques’ in […]